Embedding Palliative Approaches to Care Spread Collaborative
Only 15 percent of people in Canada have early access to palliative care at home, including residents living in long-term care homes. Sixty-two percent of people in Canada who receive palliative care receive it in an acute care hospital – most likely in the last month of their life.1
Embedding Palliative Approaches to Care (EPAC) is a proven innovation that helps staff in long-term care homes identify residents who could benefit from a palliative approach to care.
Through EPAC, team members have conversations with residents, their families and care partners about their preferences for palliative care. Together they create comprehensive, resident-centred care plans that honour the resident’s wishes, values and choices.
Early identification of care requirements plays a critical role in triggering other components of high-quality palliative care. Offering a common, consistent approach to supporting residents who are near the end-of-life creates opportunities – and provides permission – for death and dying to be openly discussed, normalized and supported.
EPAC originated from Vancouver Coastal Health’s The Daisy Project: embedding a palliative approach in residential settings, part of the open call for innovations in 2017 by the Canadian Foundation for Healthcare Improvement (CFHI – now Healthcare Excellence Canada). The following year, CFHI worked closely with Jane Webley from Vancouver Coastal Health to launch a collaborative to spread EPAC. Seven teams from five provinces and one territory participated in the collaborative until November 2019, implementing EPAC through a train-the-trainer approach in 22 long-term care homes.
How EPAC contributes to better healthcare in Canada
EPAC was part of our ongoing effort to spread and scale proven innovations that deliver high quality care closer to home and the community.
Seventy-five percent of people in Canada who have a preference would prefer to die in their home2 – including long-term care homes. By spreading EPAC, we aimed to help increase healthcare providers’ capacity and capability in delivering end-of-life care at home, as well as avoid unnecessary emergency department visits and hospital admissions.
EPAC has been instrumental in successfully shifting the culture and normalizing conversations about end-of-life and living goals. It improves end-of-life care experiences for dying residents, their families and loved ones, as well as for their healthcare providers.
Read the summary results of the collaborative
The Model
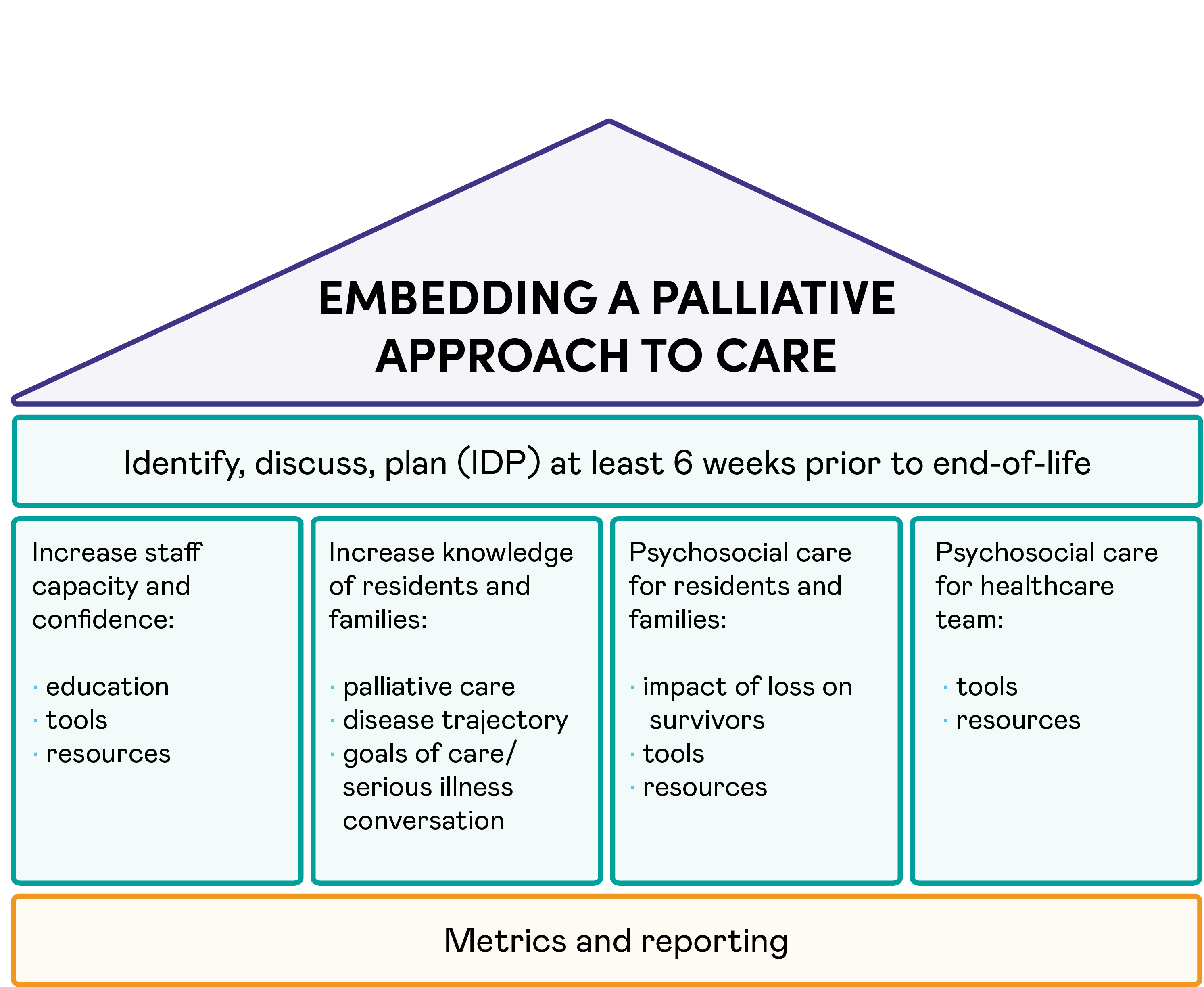
The EPAC model is a house with four pillars (shown in the diagram below) that are flexible, enabling individual long-term care homes to adopt and adapt them to their unique local needs and strengths. The overarching starting point is to identify, discuss, plan (IDP) at least six weeks prior to end-of-life. The four pillars that stand underneath this are:
- Increase staff capacity and confidence: education, tools, resources.
- Increase knowledge of residents and families: palliative care, disease trajectory, goals of care/serious illness conversation.
- Psychosocial care for residents and families: impact of loss on survivors, tools, resources.
- Psychosocial care for healthcare team: tools, resources.
Underneath the pillars sits the foundation layer of metrics and reporting.
The Approach
Through the EPAC Collaborative, we provided teams with support and access to a range of resources to help spread and embed EPAC in their long-term care homes through a train-the-trainer approach.
Long-term care providers can use our four short modules to get started in delivering palliative and end-of-life care through EPAC.
Our interactive four-part module, Giving the Gift of Time: Embedding Palliative Approaches to Care, walks long-term care teams through the journey of a real resident, offering ways to improve end-of-life care.
EPAC Teams
Haliburton Highlands Health Services, Haliburton, Ontario
Institute for Continuing Care Education and Research (ICCER), Alberta
New Brunswick Association of Nursing Homes
Parkwood Seniors Community, Waterloo, Ontario
Western Health, Newfoundland and Labrador
Yukon Health and Social Services
“Earlier conversations about things that matter provide permission for collaborative planning and saying goodbye in a meaningful way, creating lasting memories. I call this the ‘Gift of Time’ that we, as healthcare providers, can offer residents and the people that are important to them.”
Jane Webley,
Regional Leader, End of Life, Vancouver Coastal Health (2018)